Many individuals believe that freckles and dark spots are exclusive indicators of ageing, assuming that only older adults experience these skin changes. This notion is misleading; in reality, the appearance of freckles and dark spots signifies skin ageing that can occur at any age. Consequently, younger individuals may experience premature ageing, leading to a more rapid decline in skin tone, as well as the development of freckles, dark spots and hyperpigmentation. Regardless of age, the risk of developing these skin conditions increases if proper skin care is not maintained.
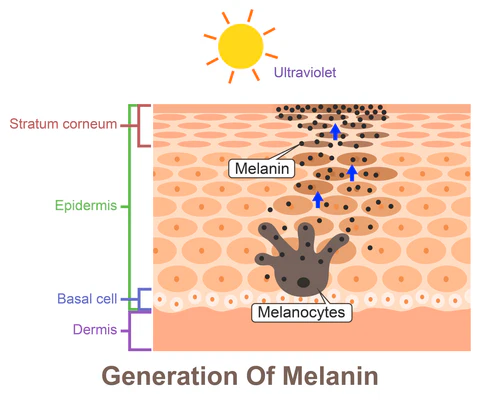
Dermatological research revealed that freckles and age spots are mainly attributed to overexposure to ultraviolet (UV) radiation, which stimulates an increase in the production of dark pigments called melanin. Melanin is a group of molecules responsible for many biological functions, including pigmentation of skin and hair as well as photoprotection of skin and eye. As melanin is produced within melanocytes, it is packaged in small, round membrane-bound organelles called melanosomes. Melanosomes are transported and positioned superficially to cell nuclei, which serves to protect from incoming ultraviolet UV-radiation.
In humans, melanin exists as three forms: eumelanin (which is subdivided further into black and brown forms), pheomelanin and neuromelanin. Eumelanin and pheomelanin are produced in various amounts in the basal layer of the epidermis within melanocytes. Neuromelanin is a dark pigment found in the brain, which has been reported to play both neuroprotective and neurotoxic roles. Have you ever wondered why there are different skin tones all over our body?
Answer: Skin pigmentation happens when melanin — the pigment that gives skin its color — builds up in tiny structures called melanosomes, found in the deepest layer of the skin’s surface (the epidermis). The color of our skin depends on the mix and amount of two types of melanin: eumelanin (which gives brown to black tones) and pheomelanin (which gives yellow to red tones). Pheomelanin is what gives a pinkish color to areas like the lips, nipples, genitals, and the glans of the penis.
Biosynthesis of Melanin
Biosynthesis melanin begins when tyrosine is converted into dihydroxyphenylalanine (DOPA), which requires tyrosine hydroxylase and tetrahydrobiopterin as cofactors. The process is catalysed by enzyme tyrosinase, which can subsequently undergo various pathways as illustrated in Figure 1:
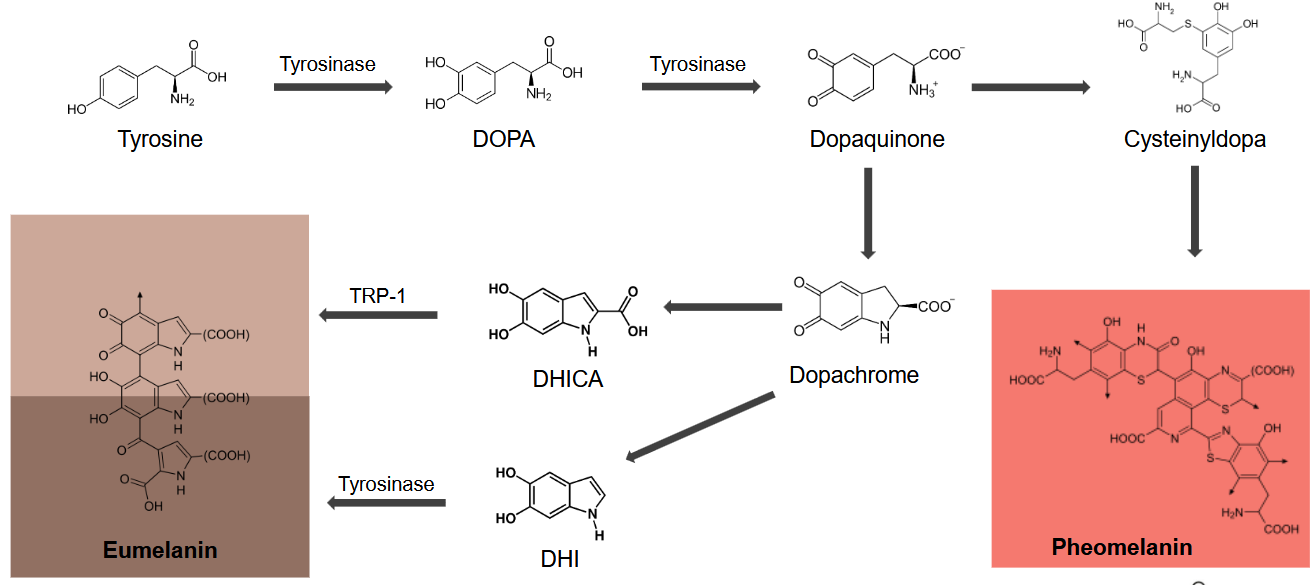
The two primary forms of melanin, eumelanin (which appears dark brown or black) and pheomelanin (which is red or yellow), respond differently to UV radiation. Eumelanin is widely recognised for its photoprotective properties. It can effectively absorb and dissipate UV rays from sunlight, thereby prevent DNA from damage and reduce the risk of skin cancer. Conversely, an overproduction of eumelanin can result in skin hyperpigmentation. Excessive melanin formed and deposited in the skin results in dark spots, patches and uneven skin tone.

Pheomelanin on the other hand can act as a photosensitizer. It is associated with phototoxic effects that can interact with UV radiation and generate reactive oxygen species (ROS). These highly reactive molecules can cause damage to cells and tissues. The increased ROS production by pheomelanin may lead to lipid peroxidation and potentially contribute to sun-induced erythema (redness) and oedema (swelling), especially in individuals with fair skin and higher pheomelanin content.
Hence, it is important to take note that although melanin plays a role as a protective barrier to the skin against UV radiation, it is not a substitute for proper sun protection. It is crucial to establish a comprehensive sun protection routine for safeguarding your skin.
Meanwhile, recent research indicates that progesterone may inhibit the proliferation of human melanocytes, thereby counteracting the oestrogen-stimulating effects. However, the effect of progesterone on melanocytes requires further investigation. Collectively, the existing findings provide valuable insights that could facilitate the development of innovative products aimed at enhancing skin tone without the need for laser treatment or toxic bleaching agents.
Skin Injuries and Inflammation
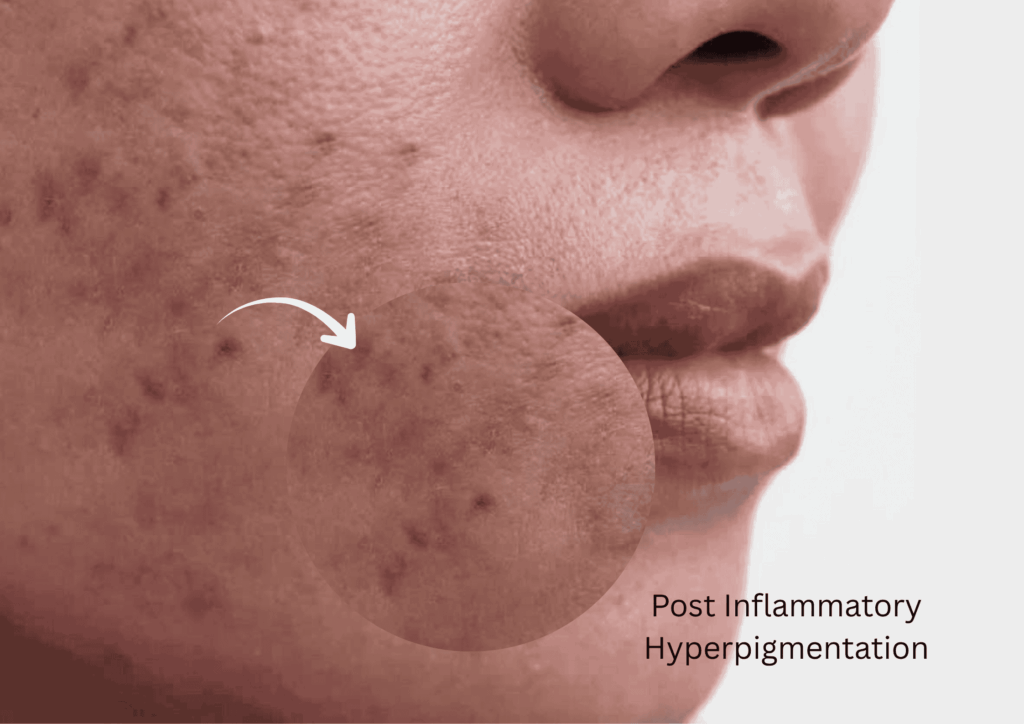
Inflammation has a significant detrimental impact on the basal layer of the epidermis, which is crucial for maintaining skin integrity and function. This inflammatory response triggers the melanocytes to release melanosomes (pigment granules). Various inflammatory mediators such as cytokines, prostaglandins and reactive oxygen species (ROS), stimulate the proliferation of melanocytes and subsequently increase the production of melanin.
The resultant condition, known as post-inflammatory hyperpigmentation (PIH), manifested as an area of increased pigmentation due to skin injuries or inflammatory events. Such events can arise from a multitude of sources, including cuts, burns, chemical exposures, acne, atopic dermatitis or psoriasis. As the skin undergoes the healing process, it often presents with a darker and discoloured appearance.
Any Solutions to Hyperpigmentation?
“Prevention is better than cure”. Addressing hyperpigmentation effectively begins with prevention; thus, establishing a sun protection regimen is essential if one has not started. Correcting skin pigmentation disorders presents challenges, primarily due to the limited availability of safe and effective treatments that can modify melanin production. The insights presented in this article indicate that:
- Inhibition of tyrosinase enzyme, which catalyses DOPA production may significantly reduce melanogenesis.
- Application of sex hormone derivatives could selectively modulate the natural mechanisms of melanin production.
- Development of topical creams containing bioactive ingredients that specifically target the skin’s pigment production pathways could offer a safer and more effective alternative to the commonly used tanning beds and bleaching creams.
Freckles and age spots are not merely signs of getting older—they reflect how our skin responds to various internal and external factors, especially sun exposure, hormones, inflammation, and the natural ageing process. At the core of these changes lies melanin, the pigment that both protects and defines our skin tone. While melanin helps shield the skin from UV damage, excessive or uneven production can result in hyperpigmentation, dark spots, and freckles.
To maintain healthy, even-toned skin, prevention is key. A consistent sun protection routine, balanced skincare habits, and awareness of hormonal or inflammatory triggers can greatly reduce the risk of pigmentation issues. Continued dermatological research and innovation in pigment-regulating skincare products also offer promising solutions for managing uneven skin tone safely and effectively. Ultimately, understanding the science behind pigmentation empowers us to care for our skin proactively—preserving its health, balance, and natural radiance at any age.
Written By: Dr. Tan Kian Meng
PhD in Engineering Technology (UTHM).M
References
- Basit H, Godse KV, Al Aboud AM. Melasma. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459271/
- Choi, W., Yin, L., Smuda, C., Batzer, J., Hearing, V. J., & Kolbe, L. (2017). Molecular and histological characterization of age spots. Experimental dermatology, 26(3), 242-248.
- Hall, P. P. (1969). The influence of hormones on melanogenesis. Australasian Journal of Dermatology, 10(3), 125-139. https://doi.org/10.1111/j.1440-0960.1969.tb01182.x
- Li, B., Mei, H., Zhou, Z., Yang, J., Zhang, Y., & Qi, F. (2024). The main causes and corresponding solutions of skin pigmentation in the body. Journal of Dermatologic Science and Cosmetic Technology, 1(2), 100020. https://doi.org/10.1016/j.jdsct.2024.100020
- Mariano, A., Bigioni, I., Scotto d’Abusco, A., Baseggio Conrado, A., Maina, S., Francioso, A., Mosca, L., & Fontana, M. (2021). Pheomelanin Effect on UVB Radiation-Induced Oxidation/Nitration of l-Tyrosine. International journal of molecular sciences, 23(1), 267. https://doi.org/10.3390/ijms23010267
- Moolla, S., & Miller-Monthrope, Y. (2022). Dermatology: how to manage facial hyperpigmentation in skin of colour. Drugs in context, 11, 2021-11-2. https://doi.org/10.7573/dic.2021-11-2
- Panzella, L., Ebato, A., Napolitano, A., & Koike, K. (2018). The Late Stages of Melanogenesis: Exploring the Chemical Facets and the Application Opportunities. International Journal of Molecular Sciences, 19(6), 1753. https://doi.org/10.3390/ijms19061753
- Schlessinger DI, Anoruo MD, Schlessinger J. Biochemistry, Melanin. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459156/
- Syder, N. C., Quarshie, C., & Elbuluk, N. (2023). Disorders of facial hyperpigmentation. Dermatologic Clinics, 41(3), 393-405.
Thawabteh, A. M., Jibreen, A., Karaman, D., Thawabteh, A., & Karaman, R. (2023). Skin Pigmentation Types, Causes and Treatment-A Review. Molecules (Basel, Switzerland), 28(12), 4839. https://doi.org/10.3390/molecules28124839